Prostatitis is characterized as inflammation of the tissue of the prostate gland, arising from the development of congestion in it.
In the modern world, it is the most common urological disease among men of all ages. According to statistics, after 30 years of age, prostatitis covers 30% of the male population, after 40 - 40%, after 50 - 50% and further in ascending order.
However, taking into account the peculiarities of diagnosis and the possibility of the course of the disease in a latent form, the real figures are much higher.

Reasons for development
Currently, the causes of the development of prostatitis are divided into two large groups:
- Infectious - (sexually transmitted infections (penetration into the tissues of the prostate of the causative agent - microbes, viruses, bacteria, fungi, etc. ): also the presence of foci of chronic infection (chronic tonsillitis, sinusitis, kidney pathology), operations on the pelvic organs andetc. ).
- Non-infectious (stagnant) (decreased immunity, hypothermia, decreased physical activity, sedentary lifestyle, prolonged sexual abstinence and vice versa excessive sexual activity, alcohol abuse, etc. ).
The development of prostatitis is facilitated by injuries, impaired blood and lymph circulation in the pelvic organs, hormonal disorders (absolute or relative androgenic deficiency).
Thus, it is emphasized that the isolated entry of the pathogen into the tissues of the organ is not always and may not necessarily be the cause of the development of the disease. The most frequently identified pathogen is Escherichia coli (86%), followed by Klebsiella, Proteus, Enterococci, Pseudomonas aeruginosa. With regard to streptococci, staphylococci, chlamydia, mycoplasma, ureaplasma, the opinions of researchers about their importance in the development of the disease differ. It is extremely rare that specific pathogens (treponema pale, Koch's bacillus, etc. ) become the causes of prostatitis.
Classification
Currently, the international classification of prostatitis has been adopted, which is the most complete and covers all types of inflammation:
- Category I. Acute prostatitis;
- Category II. Chronic bacterial prostatitis;
- Category III. Nonbacterial Chronic Prostatitis / Chronic Pelvic Pain Syndrome - a disease in which no infection is detected that lasts more than 3 months;
- Subcategory III A. Syndrome of chronic inflammatory pelvic pain (leukocytes are determined in the secret of the prostate);
- Subcategory III B. Syndrome of chronic non-inflammatory pelvic pain (there are no leukocytes in the secret of the prostate);
- Category IV. Asymptomatic chronic prostatitis (leukocytes are present in the secret of the prostate, the patient does not present complaints, the disease is detected by chance).
First signs
The main signs of acute prostatitis are an increase in body temperature and frequent urination, which is accompanied by cramps and weak pressure. In addition, signs of prostatitis include a burning sensation in the perineum and pain in the rectum during bowel movements. In the stage of purulent inflammation, spontaneous opening of the abscess and the outflow of pus from the urethra or rectum are likely.
A symptom of a chronic form is burning in the urethra and perineum, the release of pus at the end of the act of defecation or urination, increased fatigue and irritability of the body.
Difficulty urinating with prostatitis is very dangerous, which, in the absence of timely treatment, can lead to acute urinary retention. Men should not ignore such indirect signs of the development of prostatitis as a complete or partial decrease in libido, accelerated ejaculation, sometimes painful, prolonged erection at night. All these symptoms are characteristic of inflammation of the prostate gland, and even in an uncomplicated stage and amenable to adequate treatment.
Symptoms
If acute prostatitis is simply impossible not to notice, then in chronic prostatitis many do not notice certain signs or do not attach special importance to them.
Let's list the main symptoms of prostatitis in men:
- Problems with urination. Due to the narrowing of the urethra, the jet may become sluggish, thin, or intermittent. To empty, the patient has to make an effort, which should not be normal. Sometimes urine literally has to be squeezed out drop by drop, especially at the initial stage of the act of urination. Painful sensations often occur. Many patients have frequent urge to urinate (especially at night), this is due to irritation of the nerve endings. Even after going to the toilet, many have a feeling that the bladder is not completely emptied, this is due to an enlarged prostate and squeezing of the bladder. In severe cases, involuntary urine leakage or incontinence may occur.
- Painful sensations. As a rule, they are localized in the perineum, pubis or testicles, in the groin or in the lumbar region. Pain can occur suddenly and pass just as quickly, often they are quite strong, but more often there is a dull or aching character.
- Sexual problems will inevitably arise. First, libido will decrease significantly. Secondly, erection problems may occur. Thirdly, due to problems with ejaculation (ejaculation), the average duration of intercourse will change: it may become short due to early ejaculation or, conversely, too long due to delayed ejaculation. Fourthly, the sensations will also change, since the orgasm will not be bright. Fifth, the volume of semen will be significantly reduced (only a few drops may be released, which is not normal).
- Another characteristic symptom is problems with conception. If a man is planning a child, then with prostatitis, fertilization becomes impossible due to the non-viability or insufficient mobility of sperm.
- Discharge from the urethra. They are usually white in color and slimy in texture and are most common in the morning.
- In the acute course, there is an increase in body temperature (up to 38-39 °), fever, deterioration in general condition, weakness, malaise and other similar manifestations. Such symptoms of prostatitis usually appear suddenly, without any prerequisites.
In addition, many have psychological problems associated with the symptoms listed above. A man may become insecure, his self-esteem will be greatly reduced, he will be depressed or irritable and nervous. Many representatives of the stronger sex are ashamed of such delicate problems and do not consider it necessary to talk about them, keeping everything in themselves. And this puts a lot of pressure on the psyche, changes behavior and in some cases can lead to depression or a nervous breakdown.
Chronic prostatitis
Many men do not pay much attention to the manifestations of prostatitis in the early stages. These are unobtrusive painful sensations in the bladder area, frequent urge to go to the toilet. Violation of normal ejaculation and erection is associated with the stronger sex with age and is in no hurry to see a doctor. Such a frivolous attitude leads to the development of chronic prostatitis.
So, we list the common symptoms of various forms of chronic prostatitis:
- Feeling of discomfort and cuts in the urethra during urination or sexual intercourse, minor serous-purulent discharge from the urethra (mainly after prolonged urinary retention).
- Discomfort or / and moderate pain in the form of "aches" and heaviness in the perineal region, arising or worsening after drinking alcoholic beverages, physical activity, sexual intercourse. Sometimes they are transient paroxysmal in nature.
- A decrease in the ability to fertilize, which is caused by an increase in the acidity of the secretion, a decrease or lack of sperm motility, and their agglutination (gluing) by their heads.
- Sudden frequent urge to urinate (sometimes up to 3 times within 1 hour) and a feeling of insufficient emptying of the bladder, which is explained by a violation of the nervous regulation of the prostate, its muscle fibers and the bladder.
- Pain during orgasm or blurred sensations of orgasm, ejaculation disorders, expressed in its premature or, conversely, in the excessive duration of sexual intercourse. These phenomena are associated with an inflammatory process in the area of the seminal tubercle or scarring as a result of inflammation.
In order to diagnose the disease, you need to see a urologist. With the help of tests, the doctor makes a diagnosis and prescribes a course of drug treatment.
Diagnostics
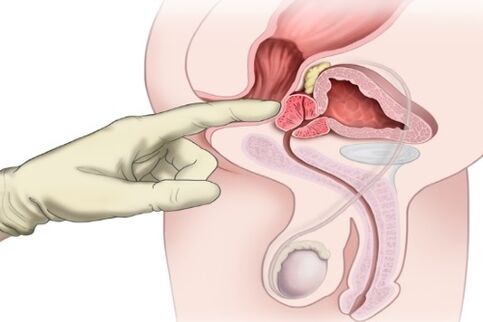
To make an accurate diagnosis, a man needs to be examined by a doctor and tested. With prostatitis, the patient experiences pain from palpation in the perineal region. Internal palpation of the rectum shows the presence of swelling in the area of the prostate gland, it becomes dense to the touch. The patient complains of problems with the genitourinary system. After collecting the anamnesis, the patient needs to pass a detailed blood test for the presence of protein surplus, increased leukocyte count and prostatic antigen.
To exclude infection, the patient must pass a smear from the urethra. The laboratory will inoculate the identified bacteria and test their sensitivity to certain types of antibiotic agents. For an accurate picture, an ultrasound examination of the pelvic organs is performed. It clearly shows inflammation and enlargement of the prostate. If the gland has grown strongly, then on ultrasound you can see the presence of residual urine in the bladder.
After all the tests and examinations passed, the man will be fully diagnosed and prescribed treatment.
Drugs for the treatment of prostatitis in men: a list
Complex treatment for prostatitis of various types may include different combinations of the following methods:
- immunocorrective therapy;
- antibiotic therapy;
- hormone therapy;
- various physiotherapy procedures;
- prostate massage;
- lifestyle change;
- surgical intervention, etc.
Treatment of prostatitis with medications includes various medications, including antibiotics:
- alpha blockers;
- hormonal drugs;
- muscle relaxants;
- immunomodulators;
- rectal suppositories;
- antibacterial drugs.
When treating with antibiotics, preference is given to fluoroquinols and macrolides, since they are able to accumulate in the required concentration in the tissues of the prostate.
- Fluoroquinols.
- Macrolides.
- Less commonly used: penicillins, cephalosporins, tetracyclines.
Prostate massage
Prostate massage shows good results. The gland receives a complex effect. First of all, it becomes possible to remove from the body the inflammatory secret that has accumulated in the prostate (it is released during the massage). Improving blood circulation through these manipulations allows you to deal with all kinds of stagnation, and also contributes to the good penetration of antibiotics into the tissue of the gland.
A set of exercises
Exercises for the prostate:
- Absolutely not a difficult exercise is used for both treatment and prevention. It consists in squeezing and relaxing the muscles of the anus. It is these muscles that are responsible for holding back the stream when urinating. Try contracting and unclenching a muscle group. This will increase the flow of blood to the area of the gland.
- Use a contrast shower to improve circulation. To do this, direct the stream of water to the perineum. First, 30 seconds of very warm water, then 10 seconds of cool.
- In the absence of acute symptoms, you can massage yourself. This is done in order to improve blood flow. The exercise is best done while lying down. The point for massage is the gap between the anus and the scrotum. Pressures should be firm, but not aggressive. The time is 3-5 minutes.
Be sure to check with your doctor before exercising. Sometimes their use is categorically unacceptable.
Immunocorrection
Decreased immunity negatively affects health.
It is this factor that is one of the fundamental in the development of the disease and its exacerbation. Long-term courses of taking antibiotics, which are mandatory for lingering prostatitis, also reduce the body's defenses. Therefore, the patient is recommended to consult with an immunologist to choose a strategy for conducting immunocorrection.
Physiotherapy
Physiotherapy for chronic prostatitis is aimed at activating blood circulation.
For this purpose, the patient is exposed to a laser, ultrasound, and magnetic vibrations are used. In some cases, these procedures are replaced with warm medicinal enemas, which are regularly given to the patient. Recommend sitz baths, mud treatment, mineral waters.
Candles
All suppositories for the treatment of prostatitis have one of the properties: relieve pain (non-steroidal drugs), relieve spasms (based on papaverine), eliminate the inflammatory process (contain an antibiotic).

Alternative methods of treating prostatitis
Treatment of prostatitis at home is carried out only with uncomplicated forms or chronic relapse. Traditional methods can increase the body's resistance to infection and relieve pain.
- Pumpkin seeds have long been used by healers in the treatment of prostatitis. They are a good and very affordable folk remedy for this condition. Since these seeds contain a lot of zinc, which is necessary for any man at any age, they quickly heal prostatitis. You just need to eat 30 seeds a day before meals. This is exactly the daily proportion of zinc for the body.
- The seeds and roots of the plant are suitable. The crushed roots of the plant are boiled for 10 minutes at the rate of half a glass of raw materials per 1 liter of water. The whole amount of the broth is drunk in even portions instead of water. The seeds are brewed in 4 teaspoons per glass of boiling water. Insist 40 minutes in a saucepan or 15 minutes in a thermos. Consume about 3-5 times a day for a tablespoon.
- The main ingredient is hazel. To treat prostatitis, you need to take either the bark or the leaves of the hazelnut. You can brew both ingredients alternately, alternating between them. Just be aware that the bark needs to be brewed twice as long as it is tougher. So, take one tablespoon of hazel leaves (or bark) and boil it in a glass of boiling water. Close the lid tightly and wait half an hour. Then strain and take 1/4 cup 4 times a day. It is better to use fresh twigs every time, but you can also use those already used several times. Usually a week of such procedures is enough - and the prostatitis goes away.
- For the treatment of the disease, candles are made, which are stored in the freezer. For the dough, take 1 teaspoon of honey, 1 egg and about 3 tablespoons of flour. The components are mixed until smooth, forming candles. Used in two courses in the morning and in the evening, 1 piece for 1 month with an interval of 10 days.
- Celandine is used with caution. The plant is poisonous, an overdose leads to severe poisoning. In parallel, the medicine from celandine will cleanse the body of polyps, neoplasms, cysts, and will prevent prostate adenoma. Freshly squeezed juice is diluted with alcohol in equal parts. Drink daily, diluting in 50 ml of water. Start treatment with 1 drop, increasing the concentration by 1 drop every day for 60 days. After 10 days, the course is repeated.
Most folk remedies are used daily 1-3 times in courses of 20-30 days. Treatment with home remedies from herbs lasts longer due to their mild effect than medication, but it is safer for the body, especially in the presence of concomitant diseases of the intestines and stomach. Treatment must be accompanied by gymnastics: raising the legs, squatting. Intensive walking is recommended for 15-30 minutes daily.

Complications of prostatitis
In the absence of timely and adequate treatment, prostatitis can be complicated by the following conditions:
- the development of chronic prostatitis;
- obstruction of the bladder;
- the development of infertility;
- recurrent cystitis;
- narrowing of the urethra;
- pyelonephritis;
- abscess of the prostate;
- sepsis.
Some of the above conditions require urgent surgical intervention!
Prevention measures
Prevention comes down to avoiding provoking factors. A healthy lifestyle, protected sexual intercourse, and the presence of one partner will reduce the likelihood of infection of the genitourinary system. General strengthening of the body and increased immune defenses are also a preventive measure for prostatitis.






























